AI tool finds sperm faster and more accurately than doctors
An artificial intelligence tool can identify sperm in severely infertile men in seconds compared to the hours it takes scientists, according to a study by University of Technology Sydney (UTS) biomedical engineering researchers.

Picture: Adobe Stock
Presenting their work at the 39th annual meeting of the European Society of Human Reproduction and Embryology (ESHRE), the study authors said the algorithm they have developed brings hope to men who want a biological child but have no sperm in their semen.
Currently, these patients must undergo a procedure where a portion of their testes is removed to help them become fathers. Embryologists extract sperm manually from this biopsy sample to fertilise the partner’s eggs through Intracytoplasmic Sperm Injection (ICSI) treatment. It can take up to six hours to find and isolate sperm in human tissue, which can undermine the embryologist’s ability to identify sperm because of mental and physical fatigue.
Data from this new study by a team led by Professor Majid Warkiani in the UTS School of Biomedical Engineering show trained AI can spare clinicians this arduous process.
Findings show the tool called SpermSearch instantly identifies sperm, then leaves the embryologist to decide whether sperm is really present and if it is viable enough for ICSI. Results show the algorithm is also more accurate than an experienced clinician.
Lead author, PhD candidate Dale Goss, said, “This tool has the ability to give patients who have very little chance of fathering their own biological children an increased chance.
“The algorithm improves antiquated approaches that have not been updated in decades. It will ensure the rapid identification of sperm in samples, which will not only increase the chance of a couple conceiving their own biological children, but also reduce stress on sperm and increase efficiency in the laboratory.”

Image courtesy Professor Majid Warkiani
Around one percent of all men have no sperm in their semen, which is the most severe form of infertility known as non-obstructive azoospermia (NOA). The condition affects around five percent of couples seeking fertility treatment.
To identify sperm for ICSI, embryologists partially shred tissue samples and tease them apart with forceps or fine needles. Any sperm present is then released into a specially prepared liquid which is placed in a petri dish.
With a microscope, the clinician searches through droplets of this liquid, a tiny portion at a time. However, contamination from other cells and particles makes this challenging. If the embryologist misses the sperm, the patient has less opportunity to become a parent, and the longer this takes, the greater the chance the sperm is not viable.
The aim of the study was to test if AI could speed up this process. The research was carried out at an IVF clinic in Sydney in two phases over five months using AI software installed on a computer. The researchers first trained the algorithm by showing it thousands of still microscope photographs. These images featured sperm and high levels of other cells and debris, but only the sperm was highlighted.
This coaching enabled the AI tool eventually to learn through image analysis what a sperm looked like using its own evaluation system that checks and adjusts its performance.
Mr Goss and his team used healthy sperm, and then samples of testicular tissue from seven patients aged from 36 to 55 years. All had been diagnosed with NOA and had already undergone surgical sperm retrieval at the clinic.
The men donated tissue left-over after treatment that had been prepared for sperm retrieval but not needed.
A test was then carried out simultaneously between the algorithm and an embryologist whose precision was considered to be 100 per cent. The researchers compared the time both took to identify sperm and their degree of accuracy.

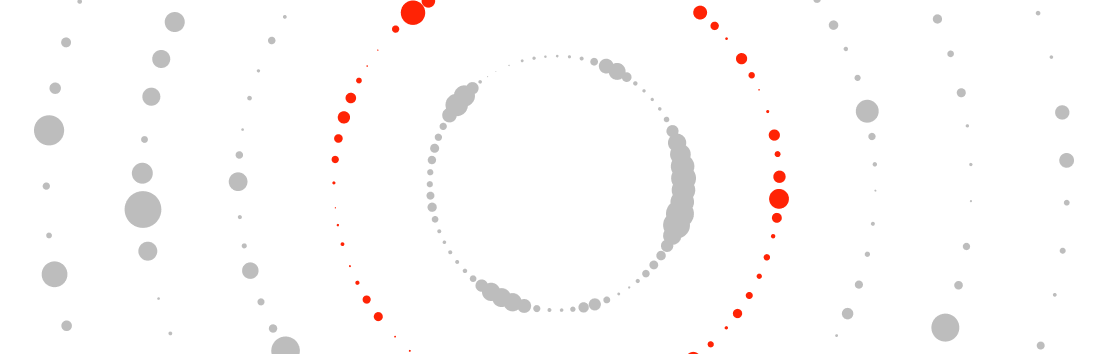
Graphic courtesy Professor Majid Warkiani
Results showed that the AI found more sperm overall, although some were only spotted by the embryologist and some by AI alone.
The embryologist found 560 sperm, the AI found 611, and between them they found a total of 688. The algorithm identified sperm for each area of droplet that it viewed in less than a 1000th of the time taken by an embryologist.
It was also more accurate and precise in identifying sperm – the AI tool found 60 more sperm, and it was five percent more accurate than the embryologist per viewable droplet area.
In their conference presentation, the authors highlight that the study is based on a proof-of-concept test and that a clinical trial is required. This is to prove the technique is useful and performs the task of sperm detection with the desired result.
They add that such research should be carried out among men with other forms of severe infertility and who are undergoing other surgical approaches, such as sperm collections from different parts of the testes.
The chair of ESHRE, Professor Carlos Calhaz-Jorge from the Northern Lisbon Hospital Centre and the Hospital de Santa Maria in Lisbon (Portugal), was not involved in this research. He said: "For men diagnosed with non-obstructive azoospermia, ICSI with sperm retrieved from the testicles is the only realistic chance of having biological children. This is a preliminary study on the use of AI for finding healthy sperm in men experiencing this type of infertility.
"Finding healthy sperm under the microscope in fragments of testicular biopsies can be an arduous process. The prospect of using AI to make the process quicker and more accurate is very interesting. We need to see more research to build on these results."
Media release from the European Society of Human Reproduction and Embryology (ESHRE)